Meet Our Researchers
A New Era of Radiotherapy
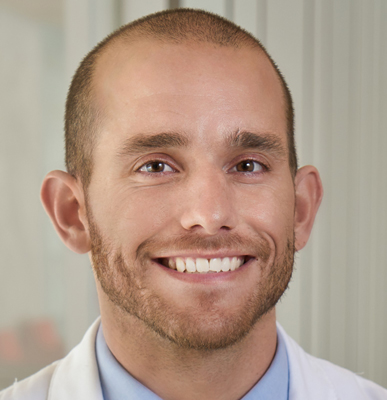
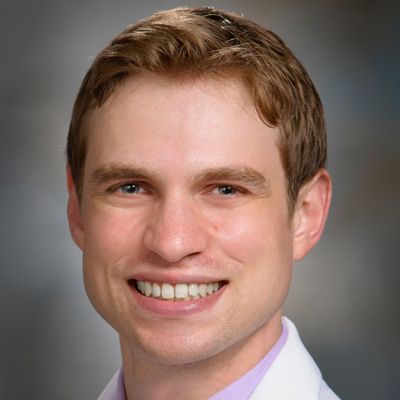
 | Nicholas Colangelo, MD, PhDDr. Colangelo and his colleagues are conducting preclinical research to investigate combining FLASH radiation therapy and a class of drugs called SOD mimetics to optimize treatment for pancreatic cancer. They aim to demonstrate that together these emerging therapies can reduce bowel toxicity, decrease tumor size and improve survival. |
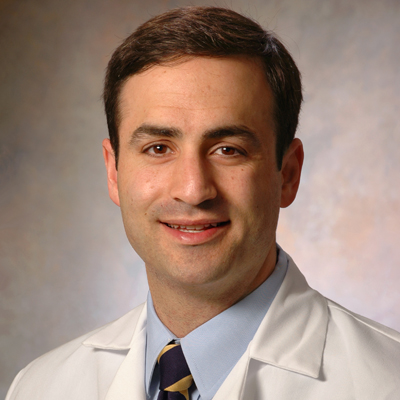
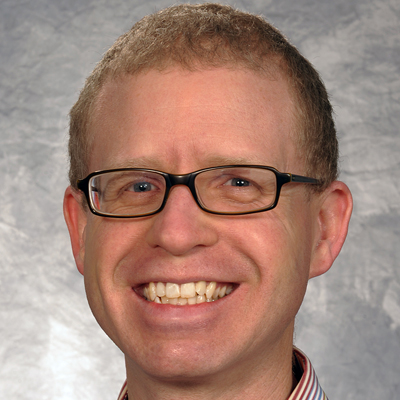
 | Michael Goldstein, MD, PhDDr. Goldstein and his colleagues are developing a FLASH RT regimen for lung cancer that consists of multiple treatments to determine whether this type of radiation delivery retains its protective effect on nearby healthy tissues. The team designed a cutting-edge platform that they are using to conduct preclinical studies on fractionated FLASH RT to help establish whether it will be safe and effective to test in clinical trials. |
 | Joseph Harms, PhDDr. Harms and his team are building and testing a new detection system to measure the dose and how fast the dose is delivered for proton FLASH RT. Their novel radiation detector uses an ultra-fast camera that will allow for real-time measurement of FLASH beams to ensure that treatments are delivered to patients as intended. |
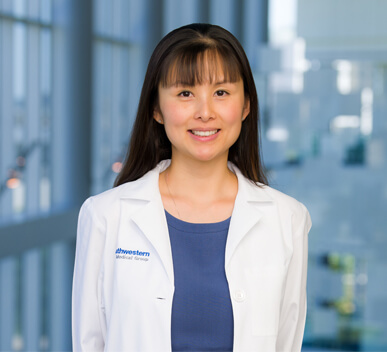
 | Katie Lichter, MD, MPHDr. Lichter and her team are conducting the first-ever investigation of wildfire events’ impact on patients with cancer undergoing radiotherapy. Their study includes surveying California-based radiation oncologists to assess their perceptions and preparedness for wildfire events. They are also analyzing care disruptions for patients receiving radiotherapy during wildfires and how exposure to such disasters affects patient outcomes. |
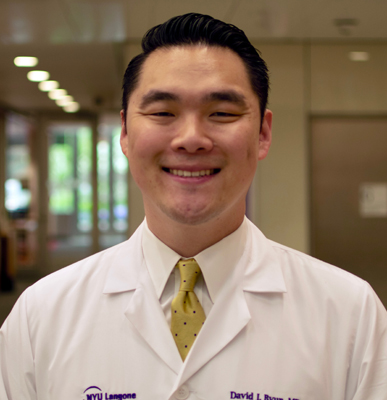
 | Michael Pennock, MD, MBiotDr. Pennock and his team are comparing three methods of delivering proton therapy for head and neck cancer, including proton pencil-beam scanning Bragg peak FLASH (PBS-BPF), a new modality they developed. They aim to determine which treatment best minimizes damage leading to side effects that jeopardize eating and speaking for patients with head and neck cancer. |
 | Ted K. Yanagihara, MD, PhDDr. Yanagihara and his colleagues are conducting a prospective clinical trial in which patients with sarcoma receive a priming dose of GRID therapy before standard treatment. They are evaluating the safety and effectiveness of adding GRID to standard treatment and investigating whether it activates an immune response that increases the number of tumor cells destroyed. |